Unraveling the Impact of Stress on Chronic Health with Theresa Piela
Unlearning Fawning and Rebuilding Self-Worth
In this week’s episode, we dive into the power of Emotional Freedom Techniques (EFT) tapping — a unique blend of traditional Chinese medicine and modern psychology. By tapping on specific meridian points while addressing emotional struggles, EFT helps release energy blockages, reducing stress, anxiety, and even trauma. 🌱✨
In this powerful episode, I sit down with holistic healing expert Theresa Piela to explore the deep connection between chronic stress and health. Theresa shares her personal story of hitting rock bottom in 2019, when chronic illness nearly led to organ failure. We dive into the guilt and exhaustion that comes with being chronically ill in a toxic world, and how healing techniques like Emotional Freedom Techniques (EFT) tapping can offer relief. 🌱✨
We’ll explore how EFT has shown promising results in mental health, from lowering cortisol levels to easing PTSD symptoms in veterans. However, with its roots in spiritual and energetic practices, EFT has sparked controversy in some Christian communities. Join us as we unpack these perspectives and discuss how EFT can be a powerful tool for both emotional and physical healing.
The Impact of Stress on the Body
Understanding Stress: Theresa breaks down the three stages of stress and how they manifest in our daily lives, leading to digestive issues and chronic illnesses. She sheds light on the silent havoc that prolonged stress wreaks on our gut health and overall bodily functions.
The Three Stages of Stress and the Fawning Response: Understanding How High-Control Religions Impact Emotional Well-Being
Stress is an inevitable part of life, but how our bodies and minds respond to it can vary significantly depending on the intensity and duration of the stressor. Hans Selye, a pioneering endocrinologist, developed the General Adaptation Syndrome (GAS) to describe the body’s physiological response to stress. This model helps explain how prolonged stress affects overall health and well-being. While the three stages of stress capture the body’s core reactions, the behavioral response known as fawning—especially common among individuals who have come out of high-control environments like fundamentalist religions—adds another layer to this discussion.
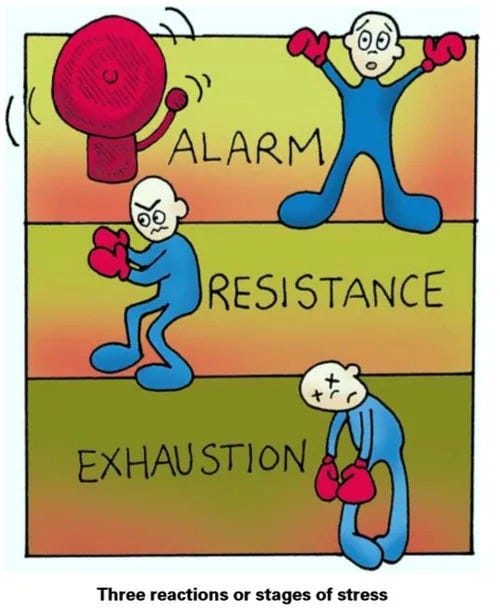
The Three Stages of Stress: General Adaptation Syndrome
Selye’s General Adaptation Syndrome describes how the body responds to stress over time, detailing three distinct stages:
1. Alarm Stage
This is the initial, immediate response to a stressor. When faced with a perceived threat, the body goes into “fight or flight” mode, releasing adrenaline and cortisol. These stress hormones increase heart rate, sharpen focus, and provide a surge of energy to prepare you to either confront the threat or escape it. In modern life, this could be triggered by anything from a work deadline to an argument with a loved one.
2. Resistance Stage
If the stressor continues beyond the initial shock, the body enters the resistance stage. While the outward signs of the fight-or-flight response might fade, internally, the body is still on high alert. Stress hormones like cortisol remain elevated, and the body tries to adapt and cope. However, this stage can’t last forever. Prolonged exposure to stress at this level takes a toll on the body, potentially leading to mental and physical exhaustion.
3. Exhaustion Stage
When stress continues for a prolonged period without adequate recovery, the body eventually reaches the exhaustion stage. Here, the body’s resources are depleted, and it can no longer function normally. Symptoms such as fatigue, depression, anxiety, and even burnout may manifest. The immune system weakens, making the individual more vulnerable to illness and disease.
Understanding these stages is crucial for recognizing when stress becomes chronic and dangerous. But there’s more to the picture when considering how stress affects behavior—especially in people who have experienced trauma or high-control environments.
Enter the Fawning Response: A Behavioral Reaction to Trauma
Fawning doesn’t fit neatly into the General Adaptation Syndrome model because it’s a behavioralrather than a purely physiological response. Still, it’s crucial to understanding how certain people cope with chronic stress or trauma, particularly in interpersonal or high-control environments.
The “Four Fs” of trauma responses—Fight, Flight, Freeze, and Fawn—describe various ways people react when they feel threatened. While fighting, fleeing, or freezing are instinctive survival responses, fawning is a more subtle and less discussed way of coping, often rooted in a need to appease the threat to maintain safety.
What Is Fawning?
Fawning involves appeasing or placating others to avoid conflict or harm. People who fawn try to please or appease the person or situation causing the stress in order to de-escalate the threat. Instead of confronting the stressor (fight), avoiding it (flight), or becoming immobilized (freeze), a person who fawns seeks to reduce the danger by submitting, people-pleasing, or over-accommodating.
This behavior often develops in individuals who have experienced prolonged stress or trauma, especially in abusive, manipulative, or high-control environments like toxic relationships or fundamentalist religions.
How Fawning Fits into the General Adaptation Syndrome Model
Although fawning isn’t a stage of stress, we can still see how it might manifest within the GAS framework:
Alarm Stage: Fawning could be an immediate response to the initial stressor. Rather than fleeing or fighting, someone might instinctively try to placate the threat. For instance, in a high-control religion, a person might conform instantly to avoid punishment or conflict.
Resistance Stage: If the stress persists, fawning can become a habitual response during the resistance stage. The person continues engaging in appeasement behaviors, attempting to manage the ongoing stressor while sacrificing their own needs and well-being in the process.
Exhaustion Stage: Over time, relying on fawning as a coping mechanism can lead to emotional and physical exhaustion. Constantly trying to meet others’ demands, avoiding conflict, and suppressing one’s own needs results in burnout and emotional depletion.
Fawning and High-Control Religions: The Long-Lasting Impact
People who come out of high-control religions often exhibit the fawning response as they attempt to navigate new environments and relationships. These religions typically operate with strict rules, strong hierarchies, and harsh consequences for dissent. As a result, members often suppress their own needs and opinions to avoid punishment or ostracism.
Even after leaving these environments, the pattern of fawning often persists. The deeply ingrained survival mechanism of appeasing authority figures to avoid conflict becomes habitual. This behavior may manifest in various ways:
People-pleasing: Going out of their way to accommodate others, even at the expense of their own well-being.
Difficulty asserting boundaries: Struggling to say no or express personal needs and preferences, often feeling guilty for doing so.
Fear of conflict: Avoiding disagreements or confrontations out of fear of rejection or punishment.
Self-silencing: Suppressing thoughts, feelings, and opinions in order to maintain harmony and avoid disapproval.
For those deconstructing from high-control religions, the fawning response can be particularly challenging to recognize and unlearn. Many may not even realize that their behaviors are rooted in a trauma response. Helping individuals understand and break these patterns is essential for their emotional recovery.
Moving Forward: Unlearning Fawning and Rebuilding Self-Worth
Breaking the cycle of fawning involves learning to assert boundaries, rebuild self-worth, and reclaim personal autonomy. This is not an easy process, especially for those who have spent years in environments where appeasement was essential for survival. Therapy, support groups, and self-compassion can be powerful tools in helping people regain their sense of self after leaving high-control environments.
By recognizing fawning as a response to trauma and stress, individuals can begin to unlearn these behaviors, reclaim their identity, and create healthier relationships—both with others and with themselves.
Understanding stress responses, both physiological and behavioral, is key to supporting individuals who are recovering from trauma. Recognizing the fawning response and how it fits into the broader stress picture can open the door to healing for those emerging from high-control situations like fundamentalist religions.
Mindset & Thought Shifting: Changing How We React to Stress
We must first accept that stress is a normal and natural part of life. Short-term stress, when followed by ample recovery, can enhance cognition and boost our capabilities. It’s like strength training: with proper recovery, the stress we place on our muscles leads to gains. However, persistent stress, if not managed properly, can be damaging. This is why we must shift our relationship with stress.
In times of severe depletion and exhaustion, recovery takes time and commitment. Start by meeting yourself where you are. Shift your mindset by deliberately choosing thoughts that signal to your body that everything is okay. Surround yourself with calming influences—whether it’s people, sounds, colors, or landscapes—that make you feel safe and hopeful. This isn’t a luxury; it’s a requirement for healing. Equally important is removing stimuli that drain you and recognizing that your body has an incredible capacity to heal when given the right tools.
As the Dalai Lama once said, “If a problem is fixable, if a situation is such that you can do something about it, then there is no need to worry. If it’s not fixable, then there is no help in worrying. There is no benefit in worrying whatsoever.”
Fuel & Nutrition: Supporting Your Body’s Adaptive Stress Response
Just as important as shifting your mindset is fueling your body with the right nutrients. A starved or inflamed system will struggle to adapt to stress, especially when trying to balance internal chaos. Proper nutrition is key to supporting the body’s stress response.
When the body isn’t fueled properly, persistent stress leads to harmful effects, such as blood sugar swings, hormonal dysregulation, and weakened immunity. To counteract this, we need to provide the body with the building blocks it needs to recover.
Here’s a high-level look at what your body requires for optimal function:
Proteins: Anti-inflammatory sources like grass-fed beef, broths, shellfish, and dairy.
Carbohydrates: Glucose and fructose from fruits, honey, maple syrup, and root vegetables.
Fats: Saturated fats are essential.
Vitamins & Minerals: Vitamin C, D, E, B1, B6, B12, calcium, magnesium, copper, sodium, potassium, selenium, and zinc.
Addressing intestinal permeability, blood sugar imbalances, and other stress-induced dysfunctions through proper nutrition will help rebuild resilience. For those with severe gut issues, a nutrient-dense, elimination-style diet—like carnivore plus easy-to-digest carbs—may be necessary short-term to restore balance.
In the end, listening to your bodyis critical. Experiment with what makes you feel good, trust yourself, and remember: you know best.
By shifting your mindset and supporting your body with proper fuel, you can navigate life’s stressors with resilience and strength.
Ever wonder why stress keeps you up at night?
Sleep Disruption and Hormones: How Stress, Trauma, and Hormonal Imbalances Impact Sleep Quality
Sleep is one of the most critical factors for overall health, and yet, it’s often disrupted by stress and hormonal imbalances. In this section, we’ll dive into how stress hormones like cortisol and adrenaline interfere with sleep, explore the impact of early life trauma on sleep quality, and discuss how the menstrual cycle and hormonal imbalances can further complicate our ability to achieve restful sleep.
Stress Hormones and Sleep Disruption
Stress hormones such as cortisoland adrenaline play significant roles in the body’s response to stress, but when they’re constantly elevated, they can wreak havoc on our sleep.
Cortisol: Often referred to as the “stress hormone,” cortisol follows a natural rhythm called the circadian rhythm. In healthy individuals, cortisol levels are highest in the morning to help us wake up and get ready for the day, and they naturally decline in the evening to prepare the body for rest. However, when we are under chronic stress, cortisol can become dysregulated. Instead of dropping at night, elevated cortisol levels can keep us in a state of alertness, making it difficult to fall asleep or stay asleep. This leads to frequent waking, shallow sleep, and feeling unrefreshed in the morning.
Adrenaline (Epinephrine): Adrenaline is the hormone responsible for the fight-or-flight response, which prepares the body to face a threat by increasing heart rate, blood flow, and energy levels. If adrenaline surges before bed—due to stress, anxiety, or even unresolved trauma—it can make falling asleep nearly impossible. You might feel restless, agitated, or have racing thoughts, all of which disturb the calm necessary for a good night’s sleep.
Practical Strategies for Managing Stress Hormones for Better Sleep
Create a Wind-Down Routine: Establishing a relaxing pre-sleep routine helps signal to your body that it’s time to rest. This can include dimming lights, turning off electronic devices (which emit blue light and can increase cortisol), and engaging in calming activities like reading, gentle stretching, or meditation.
Balance Blood Sugar: Blood sugar spikes and crashes can trigger cortisol release. Eating a well-balanced meal with protein, healthy fats, and complex carbohydrates before bed can stabilize blood sugar levels and prevent cortisol surges during the night.
Supplement Support: Some supplements, such as magnesium, have been shown to help reduce cortisol levels and promote relaxation. Herbal adaptogens like ashwagandha and holy basil can also support the body’s stress response and reduce cortisol.
Mind-Body Techniques: Practices like yoga, deep breathing exercises, and progressive muscle relaxation can help lower cortisol and calm the nervous system before sleep.
The Impact of Early Life Trauma and Adverse Events on Sleep
Early life trauma or Adverse Childhood Experiences (ACEs)have profound effects on the body’s stress response systems, which can manifest later in life as sleep disturbances. Research shows that people who have experienced trauma, particularly in early development, often have overactive sympathetic nervous systems and altered cortisol levels, leading to difficulty achieving deep, restorative sleep.
Hypervigilance: Trauma survivors often experience hypervigilance, a heightened state of awareness where the body is constantly scanning for potential threats, even during sleep. This state of heightened arousal makes it hard to relax, and the individual may have trouble entering deeper stages of sleep like REM (Rapid Eye Movement) or slow-wave sleep.
Fragmented Sleep: Those with a history of trauma may wake frequently during the night, as their bodies remain on high alert. This fragmentation prevents the deep, uninterrupted sleep necessary for physical and emotional recovery.
Nightmares and Flashbacks: Trauma-related nightmares are common and can disrupt sleep, causing the individual to wake in distress. Flashbacks, even during waking hours, can trigger the body’s stress response, elevating cortisol and adrenaline and making sleep difficult.
Strategies to Address Sleep Disruption in Trauma Survivors
Trauma-Informed Therapy: Engaging in trauma therapy, such as Cognitive Behavioral Therapy for Insomnia (CBT-I) or Eye Movement Desensitization and Reprocessing (EMDR), can help individuals process traumatic memories and regulate their nervous system responses, ultimately improving sleep.
Grounding Techniques: Practicing grounding exercises, such as focusing on your breath or engaging your five senses, can help bring your body back into the present moment, reducing hypervigilance and promoting relaxation before bed.
Sleep-Friendly Environment: Creating a sleep environment that feels safe and secure is crucial for trauma survivors. Using weighted blankets, soothing sounds, and minimizing noise or light disturbances can enhance feelings of safety during sleep.
The Role of Menstrual Cycles and Hormonal Imbalances in Sleep Disruption
For many women, sleep disturbances can be closely tied to the fluctuations in estrogen, progesterone, and other hormones that occur throughout the menstrual cycle. Hormonal imbalances, especially during perimenopause or menopause, can further exacerbate sleep issues.
Estrogen and Progesterone: These hormones play vital roles in regulating sleep. Estrogenpromotes sleep by increasing serotonin, a neurotransmitter that helps regulate mood and sleep patterns. Progesterone has a calming, sedative effect on the brain and helps prepare the body for sleep. However, imbalances in these hormones—whether due to the menstrual cycle, pregnancy, or menopause—can lead to insomnia, night sweats, and difficulty staying asleep.
Premenstrual Sleep Disruption: Many women experience disrupted sleep in the luteal phase of their cycle (the days leading up to menstruation), when progesterone levels spike and then rapidly drop. This sudden shift can lead to insomnia or restless sleep, often accompanied by PMS symptoms like bloating, mood swings, and cramps.
Perimenopause and Menopause: As women approach menopause, declining estrogen and progesterone levels can lead to hot flashes, night sweats, and other symptoms that interfere with sleep. The lack of estrogen can also cause vaginal dryness and discomfort, further disrupting rest.
Cortisol and Menstrual Cycles: High cortisol levels, often due to stress, can also impact the menstrual cycle by suppressing the release of sex hormones, leading to irregular periods or exacerbating PMS symptoms, which in turn disrupt sleep.
Practical Strategies for Hormonal Sleep Issues
Track Your Cycle: By tracking your menstrual cycle, you can become more aware of patterns in sleep disturbances and adjust your habits accordingly. For instance, you might prioritize stress management techniques and good sleep hygiene during the luteal phase.
Herbal Support: Certain herbs like chasteberry(Vitex), black cohosh, and red clover can help balance estrogen and progesterone levels, potentially reducing sleep issues related to PMS or menopause.
Hormone Replacement Therapy (HRT): For women in perimenopause or menopause, bioidentical hormone replacement therapy (BHRT) can help restore hormone balance, improving sleep quality. Consulting a healthcare provider about HRT options may be helpful.
Takeaway: Supporting Hormonal Balance for Better Sleep
Stress, trauma, and hormonal imbalances each play a major role in sleep disruption, but by managing stress hormones, addressing trauma, and supporting hormonal health, you can improve your ability to achieve deep, restorative sleep. Prioritizing sleep hygiene, engaging in calming practices, balancing blood sugar, and supporting hormone levels with natural or medical interventions are key strategies in restoring balance and reclaiming restful nights.
Nutritional and Lifestyle Adjustments: Theresa shares actionable tips on how to nourish your body for better sleep. From balancing blood sugar to enjoying nutritionally dense meals, she emphasizes the importance of tuning into what your body needs, rather than following rigid dietary rules. We also explore the benefits of bedtime snacks like fructose, carbs, and chamomile tea to promote restful sleep.
Emotional Resilience and Self-Compassion: In a world that demands so much from us, Theresa encourages us to meet ourselves with curiosity and compassion. She reminds us that it’s okay to feel frustrated, angry, or tired—these emotions are part of being human. Through self-experimentation and treating ourselves with the kindness we would offer a child, we can navigate the healing journey with more grace.
Tune in to this episode for a heartfelt and insightful discussion that will leave you with practical tools and a renewed sense of hope on your path to healing. Whether you’re struggling with insomnia, chronic stress, or just trying to find balance in a chaotic world, Theresa’s wisdom is not to be missed.
For helpful tapping videos, be sure to check out TappingwithT.com, where you can explore a variety of free resources without needing to sign up. You can also take advantage of a 7-day free trial to the membership and app! Additionally, if you’re interested in personalized support, 30-minute discovery calls are available for those considering 1:1 sessions.
About Us — Living Roots Wellness
The Trauma-Brain-Gut Connection — Living Roots Wellness
Stress, Adaptation, & Repair — Living Roots Wellness
EFT Tapping — Living Roots Wellness
#EFTTapping #ChronicStress #HolisticHealing #Spirituality #deconstruction